EFFECT OF TETRA-ATAXIOMETRIC POSTUROGRAPHY PROGRAMS (TETRAX) ON STROKE PATIENTS WITH IMPAIRED STANDING BALANCE
SALT Journal of Scientific Research in Healthcare
Volume 2, Issue 1, Page 20-30, Published on 13th Feb 2022
https://doi.org/10.56735/saltjsrh.ms2202012030
Research Article
*BHAWNA SHARMA1, PRATEEK GAUR2, POONAM KADIAN3
1Assistant Physiotherapist, ITS Institute of Health and Allied Sciences, Muradnagar, U.P.-201206, India
2Sr. Consultant and Head- Rehabilitation Department, VIMHANS Hospital, Delhi-11006, India
3Senior Clinical Investigator, Optum Global Solution, UHG, Hyderabad, India
Corresponding Author: Dr. Bhawna Sharma, ITS Institute of Health and Allied Sciences, Muradnagar, Uttar Pradesh 201206, India.
ORCID ID: 0000-0002-8554-2516
Email: [email protected]
ABSTRACT
Patients are suffering from stroke experience balance dysfunction leading to poor weight shifts and reduced weight bearing on the affected lower limb. The Tetrax biofeedback system is a Centre of Pressure-controlled, video game-based exercise system designed for patients with balance dysfunction. Objective: This study aimed to investigate the effects of using Tetrax balance games and conventional rehabilitation on the balance and mobility of subjects with impaired standing balance due to stroke. Design: Pretest-posttest Randomized Clinical Trial Method: A total of thirty patients (including male and female) who have suffered a stroke at least six months back, diagnosed with hemiplegia within the age group of 35-65 years with MMSE Score = 24 were recruited. Six subjects did not give their consent. Subjects were assigned to Group 1 (test group) and Group 2 (control group), using Convenience sampling. Group 1 (test group) consisted of 12 subjects (both male and female) and received conventional therapy and tetrax sessions. Group 2 (control group) consisted of 12 subjects (both male and female) and received only conventional therapy. All participants received conventional outpatient rehabilitation therapy (which accounted for an average of 60 minutes of physiotherapy for the control group and 40 minutes for the test group per day) three days a week in an outpatient setting. The test group received additional Tetrax biofeedback balance training three days per week (20 minutes per day) for four weeks in the same outpatient setting. The Tetrax system was equipped with four independent force plates under the toes and heels. The outcome measures of the study were BBs and FIMS. All outcome measures were evaluated pretest and posttest. Result: The means standard deviations of Improvement in BBS in test and control groups are 3.83 4.64 and 1.25 1.28, respectively. On applying the t-Test, we found the mean difference of 0.077 of Improvement in BBS in the test and control group is not significant. The means standard deviations of Improvement in FIMS in test and control groups are 2.83 2.24 and 1.75 1.21, respectively. On applying the t-Test, we found the mean difference of 0.156 of Improvement in FIMS in the test and control group is not significant. Conclusion: The current study found that both groups—those receiving only conventional therapy and those receiving a combination of tetrax and conventional therapy—improved their balance significantly, although there was no significant difference between them.
Keywords: Stroke, Tetrax, Balance, Weight shift in lower limbs, Postural Balance.
INTRODUCTION
World Health Organization defines stroke as rapidly developing signs of focal or global disturbance of cerebral functions, lasting more than 24 hours or leading to death, with no apparent causes other than a vascular origin.1
Stroke is a leading cause of disability among adults in many developed countries.2 Stroke is the third most common cause of death and the most common cause of long term adult disability in the western world.3 It is among the leading causes of mortality and morbidity in India. The prevalence rate of stroke in India varies across regions, 84-262/100000 in rural areas and 334-424/100000 in urban areas. The incidence rate is 119-145/100000 based on recent population studies.4
Major risk factors causing stroke are hypertension, heart diseases and diabetes. This coexistence of vascular problems increases significantly with the patient’s advancing age. 5,6 The hampered blood supply causes a stroke to the brain because an artery supplying to the brain is blocked (ischemic stroke) or bursts (hemorrhagic stroke), disrupting the brain tissue.7
Depending upon the pathology, stroke is classified as ischemic and hemorrhagic stroke.1 The Indian Collaborative Acute Stroke Study (ICASS), a recent study conducted among 2162 admitted stroke patients across India, recorded 77% of patients suffering from ischemic stroke, 22% from hemorrhagic stroke and 1% cases of unspecified stroke.5
Common stroke symptoms include problems in walking, loss of balance and coordination, aphasias, dizziness, numbness, weakness or paralysis, blurred, blackened or double vision, sudden severe headache, confusion, stress or depression. Hemiparesis is the most common neurological deficit post-stroke. Damage to the descending tracts of the nervous system results in abnormal regulation of spinal motoneurons, causing altered postural and stretch reflexes and voluntary movement.8, 9, 10, 11
Tools available to examine the patient for risk of stroke and diagnose an in action stroke include- physical assessment of the patient, ultrasonography, arteriography, CT scan, MRI, CT and MRI with angiography, echocardiography.12
Medical treatment and rehabilitation are equally important parts of the treatment to be administered to a patient who has suffered a stroke. The rehabilitation process should include speech therapy, occupational therapy, physical therapy, and family education. Early rehabilitation, specifically mobilisation, helps in preventing or reducing the harmful effects of deconditioning and the risk for the secondary impairments.13
Rehabilitation may also include target-specific training, enriched environment, CIMT, BWSTT, robotic training, strength training, ABTs, self-actualisation, TENS, multisensory feedback, action observation, VR and music therapy.13, 14, 15
Loss of balance and mobility affect the quality of life of post-stroke individuals to a greater extent.8 Ability to distribute weight evenly (postural symmetry) and to shift weight according to the task requirements is most important to maintain normal balance.16
The balance consists of three main ingredients: steadiness, symmetry, and dynamic stability. The capacity to hold a certain posture with minimal deviating movement is known as steadiness (sway). The term symmetry is equal weight distribution between the weight-bearing components (eg, the feet in a standing position, the buttocks in a sitting position), and dynamic stability is the ability to move without losing balance. These three components of balance (steadiness, symmetry, and dynamic stability) get disturbed after a stroke.17
Integration of information from three sensory modalities: somatosensory, visual, and vestibular afferents, is essential for adequate postural control. Sensory information is regulated dynamically and modified with variable environmental conditions.9
Posture control is essential in maintaining balance in daily living activities (ADL).18 New techniques to treat balance impairments and associated problems such as postural impairments and difficulty in performing ADLs, as a complement to traditional rehabilitation approaches, have been used to work on these impairing features and increase motivation and intensive training, such as virtual reality and Tetrax.
Through force plate systems, visual biofeedback training provides extrinsic information about task progression to the patient via a computer screen and improves motor learning.19 During feedback training, a goal is set, and the performer uses feedback to discover performance errors by comparing their movement to the expected goal and trying to improve the next attempt.
Visual feedback and feedback regarding weight distribution and centre-of-pressure is effective in increasing stance symmetry.20 Postural reactions can be quantified in situations of reduced stability on force platforms. Pressure cells have been incorporated into force platforms to measure oscillations that cannot be detected by the human eye.9
Lack of interest in conventional exercise programmes lowers the effectiveness of the therapeutic exercise.19 Some video games, which are classified as non-immersive virtual reality systems, are built with the relevant concepts of neuroplasticity. The use of the centre of pressure (COP)-controlled exercise protocols designed in games has been reported to improve subjects dynamic balance control.19,21
Virtual reality is described as the use of interactive simulations created using computer hardware and software that allow patients to interact with things and events that appear and feel genuine.7
Tetrax is Tetra-Ataxiometric Posturography Program. Tetrax makes use of visual feedback and force platform systems. Tetrax is a system designed to accurately examine balance and stability non-invasively, pinpoint their source and also provide balance training for patients. Tetrax has become an important focus of overall health for patients with a wide range of problems, owing to its user-friendliness and accurate, non-invasive testing. 22
The Tetrax biofeedback system is a COP-controlled exercise system working on designing video games prepared for patients with balance dysfunction. A traditional force platform biofeedback system includes at least two force plates for weighing each foot, a monitor to display the COF or COP, and software with training methods and data analysis capabilities. Some units also provide auditory and visual feedback in response to the unsatisfactory performance.17
Tetrax is the only system available that measures balance at four different points, each separate yielding signals of pressure variations. This allows the analysis of sway patterns for each four-foot part and how they interact. These balance parameters, which provide essential diagnostic information for the physician to calculate the fall risk index, are not available on any other posturographic device.22
RESEARCH QUESTION
Is the Tetra-Ataxiometric Posturography program more effective in improving balance than the conventional rehabilitation program in post-stroke patients?
METHODS
Study Design: Pretest-Posttest Randomized Clinical Trial.
Sample: Sample size- 24 post-stroke patients from VIMHANS hospital and Neurophysiotherapy OPD of ITS Paramedical College, Muradnagar based on inclusion and exclusion criteria.
Source of Data: Neurophysiotherapy OPD of ITS Paramedical College, Muradnagar and VIMHANS hospital, Nehru Nagar, New Delhi.
Sampling: Subjects were assigned to Group 1 (test group) and Group 2 (control group), using Convenience sampling.
Inclusion Criteria: Age should be between 35 to 65 years, the stroke of more than six months duration. The subject should follow and obey the commands of the physiotherapist. MMSE score = 24. The subject did not have any experience in Tetrax balance games. The subject should be able to stand.
Exclusion Criteria: Any other neurologic condition, Cardiac instability with cardiac symptoms, Uncontrolled blood pressure, Chest pain in24 hours prior to the initial assessment, Presence of cardiac arrhythmia and signs of DVT, Joint deformities like osteoarthritis etc., Significant orthopaedic and chronic pain, Active neoplastic diseases, Severe pulmonary disease, Speech aphasia.
INSTRUMENTATION
Sensory assessment kit, goniometer, reflex hammer, MMSE scale, berg balance scale, FIM scale, therabands, weight cuffs, swiss ball, wobble board, parallel bar, Tetrax apparatus, pen, pencil, paper
PROTOCOL
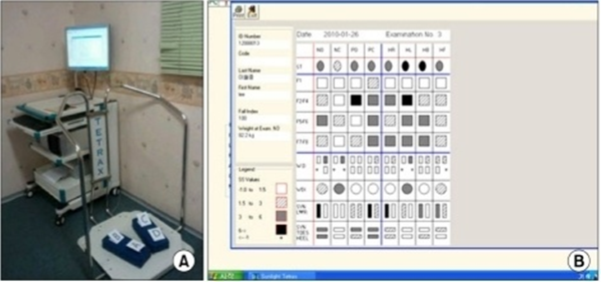
A total of 24 subjects were divided into two groups. Group 1 (test group) consisted of 12 subjects (both male and female) and received conventional therapy and tetrax sessions. Group 2 (control group) consisted of 12 subjects (both male and female) and received only conventional therapy. All participants received conventional outpatient rehabilitation therapy (which accounted for an average of 60 minutes of physiotherapy for the control group and 40 minutes for the test group) three days a week in an outpatient setting. In the same outpatient environment, the test group received additional Tetrax biofeedback balance training thrice a week (20 minutes per day) for four weeks. The Tetrax system was equipped with four independent force plates under the toes and heels (Figure 1). The foot pressure was acquired via each force plate. An interface box captured the data from the force plates for display on a personal computer, which contained the Tetra biofeedback games software. The video games were controlled via the change in the player’s COP. The Tetrax biofeedback exercise system included 11 games. Four games were chosen based on common balance deficits after a stroke. The therapeutic goals included achieving even weight distribution and improvement in right-left and front-back weight transfer. The following four games were chosen to improve balance:
1. Catch: Catch one ball by moving the other ball. The movable ball is moved by changing the pressure of the patients’ feet.
2. Skyball: Move the baseball glove by using the right-left movement of the patient’s feet to catch the baseballs.
3. Gotcha: Move the bowling pins by using the right-left movement of the patient’s feet to avoid the bowling balls.
4. Speedball: Move the basketball hoop by using the front-back movement of the patient’s feet to catch the basketballs.
OUTCOME MEASURES
Berg Balance Scale and Functional Independence Measurement Score.
DATA ANALYSIS
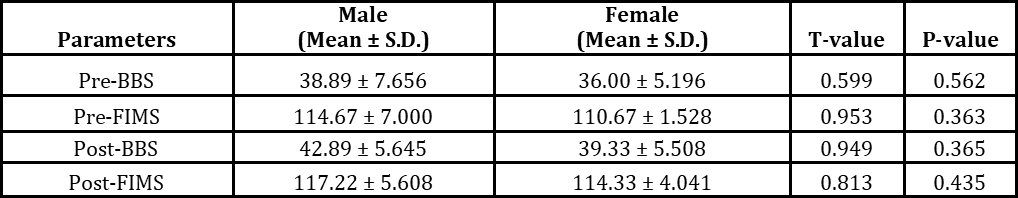
All the data was collected and analysed. The independent variables analysed were age and gender. The data were analysed using a statistical package for social sciences SPSS 16.0. The normality of data was tested by the Shapiro-wilk test, and we found the data is normally distributed. All variables are expressed as mean, standard deviation, SEM, and 95% C.I.A paired t-Test was used for dependent variables (intra-group comparison), and an unpaired t-test was used to test the significance of different variables between two different groups. The significance level and confidence intervals were 5% and 95%, respectively.
RESULTS
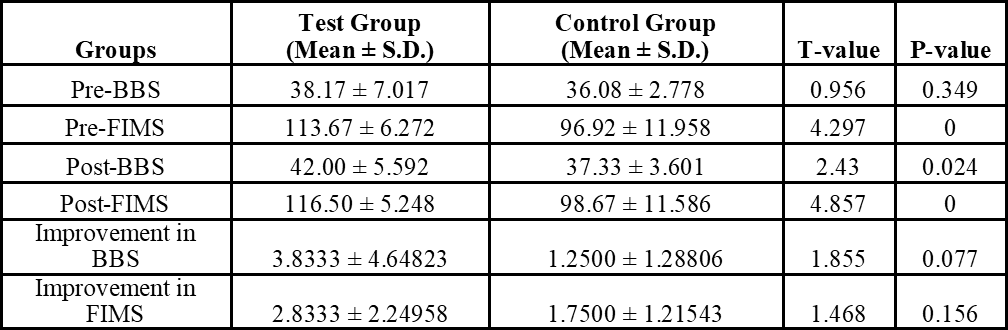
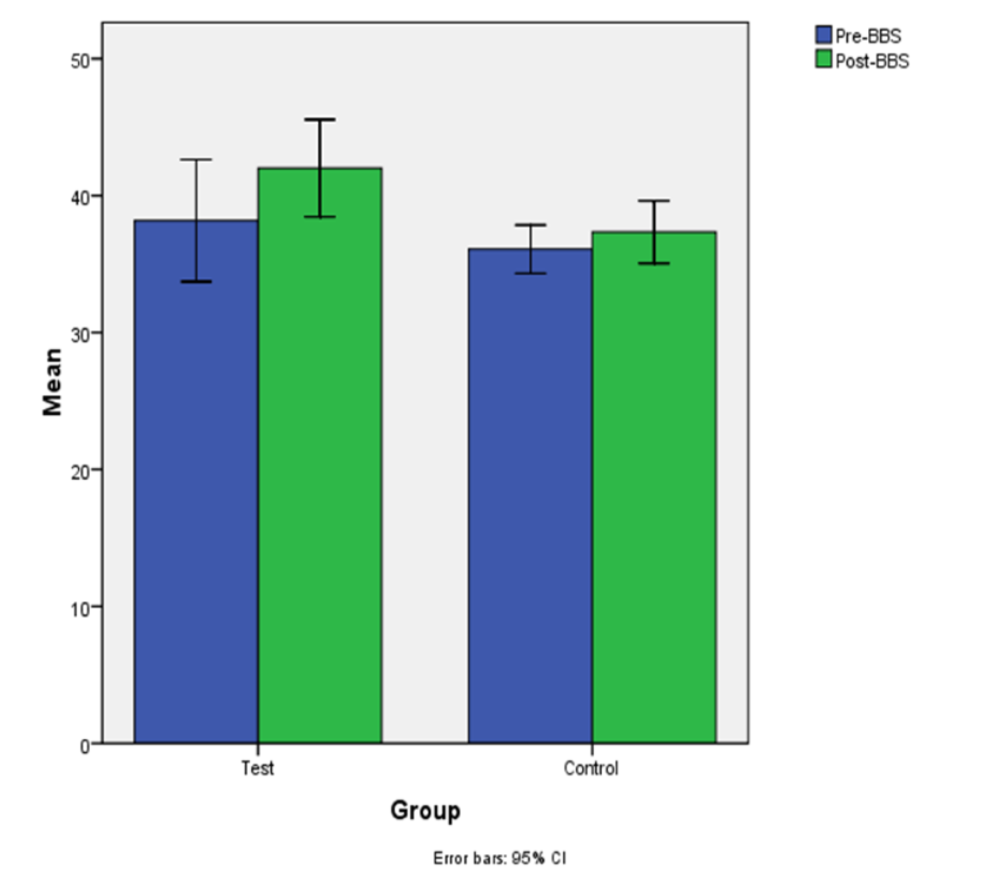
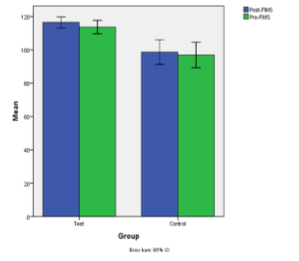
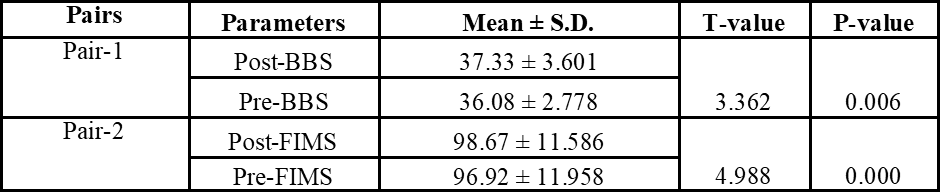
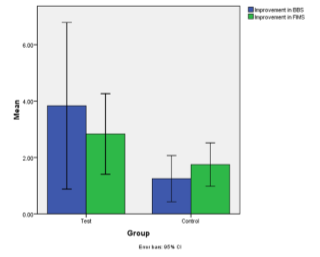
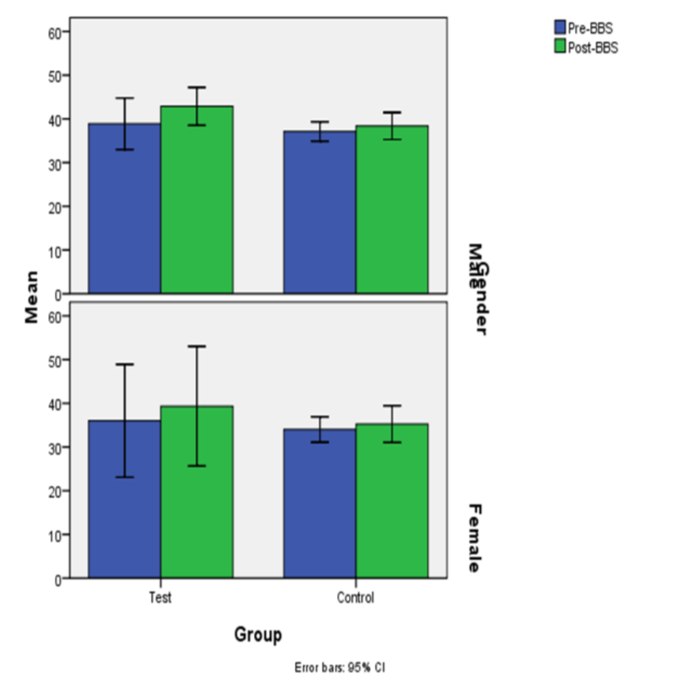
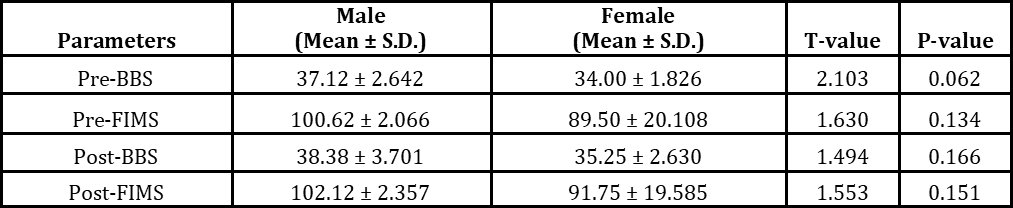
This section deals with presenting the data once collected information is tabulated and analysed using appropriate analysis tools. The means standard deviations of Improvement in BBS in test and control groups are 3.83 4.64 and 1.25 1.28, respectively. On applying the t-Test, we found the mean difference of 0.077 of Improvement in BBS in the test and control group is not significant (p> 0.05) (Table 5.1). The means standard deviations of Improvement in FIMS in test and control groups are 2.83 2.24 and 1.75 1.21, respectively. On applying the t-Test, we found the mean difference 0.156 of Improvement in FIMS in the test and control group is not significant (p> 0.05) (Table 5.1).
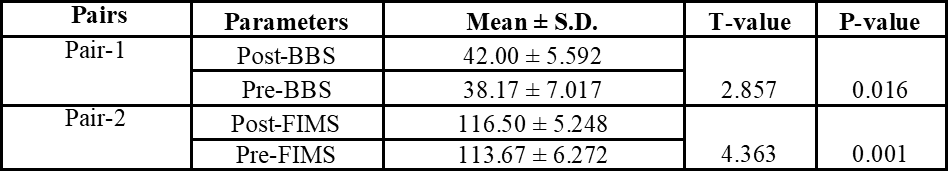
On applying paired t-Test to the mean and standard deviation of Pre- Post- BBS and FIMS in the test group, we found mean difference between PostBBS PreBBS and PostFIMS PreFIMS is significant ( p<0.05) (Table 5.2).
On applying paired t-Test to the mean and standard deviation of Pre- Post- BBS and FIMS in the control group, we found mean difference of PostBBS PreBBS and PostFIMS PreFIMS is significant ( p< 0.05 ) ( Table 5.3 ).
DISCUSSION
The study was aimed to investigate the effect of Tetrax balance trainer on balance in post-stroke patients. On analysis, the result revealed that there was a non-significant difference between the group that received a combination of conventional and tetrax sessions and the group that received only conventional therapy. The improvement in BBS and FIMS is insignificantly greater in the test than in the control group, and it may be significant if we increase our sample size. The results revealed a significant difference within groups but not significant between the groups. The people with stroke who participated in this study demonstrated marked improvements in their balance abilities over time. Our findings suggest that Tetrax balance game training is a feasible and effective intervention for patients with chronic stroke. All subjects improved postural and activity-based balance ability, with no added benefit associated with the introduction of Tetrax balance games. Research has been published favouring intensive and repetitive task-specific training for functional recovery after a stroke.19 However, conventional repetitive exercises usually cause patients to lose interest. Lack of interest can decrease the potential effectiveness of the therapy. The engaging nature of the game-based approach may increase motivation and repetitive practice. Participants enjoyed a lot while training with the games. Since Tetrax games were not as diverse as commercial entertainment systems, some participants lost interest in playing the games at the late stage of the intervention. The Tetrax training is advantageous and favourable due to stimulation of the static balance control.23
Song et al. performed a study to explore the effect of virtual reality (VR) and a tetra-ataxiometric posturography (Tetrax) program on stroke patients with compromised standing balance.24 It is the first study investigating adding VR and Tetrax to conventional training. The BBS and FIM scores were improved in all groups, with no significant differences between groups.
In our study, both groups participated in a total therapy time (60 minutes), which only differed with the type of intervention. This aspect has provided the possibility to examine the effectiveness of a conventional mixed program (Tetrax + conventional physiotherapy) compared to conventional physiotherapy. Our findings differ from the study by Hung et al. (2016)19 that found the greater effectiveness of outcomes in favour of Tetrax, but the intervention time was different in his study, which can evidence the effect of the training volume offered. Our results demonstrate that equating the groups according to the total time of training received by the conventional physiotherapy group and the combined group that received both conventional physiotherapy and Tetrax session; the effects are similar. We found that training with Tetrax resulted in improved symmetric weight-bearing. Games were selected to enhance weight-bearing on an affected limb, such as Gotcha and Speedballs. The Skyballs game also enhanced Antero-posterior balance. Weight-bearing in different directions improved with the Catch the Green Ball game. Proprioception of the affected limb also improved in the affected limb after training with Tetrax. This effect was due to repetitive weight shifting during the training course that increased joint compression, improving proprioceptive feedback.
There is a question as to why subjects receiving additional Tetrax balance training failed to outperform another group. We concluded that practice is believed to be essential for effective learning of complex tasks, and the training should resemble real-life tasks as much as possible.
No falls were reported during Tetrax sessions. However, 1 of the patients of the test group reported having mild pain in his lower limb and buckling of the knee, possibly as a result of repeated weight shifting movements. Stretching exercises were recommended before each Tetrax biofeedback balance training session.
BBS and FIMS are used as assessment instruments in our study. The BBS was designed with the explicit intention of providing a means to determine the change in balance ability over time. The reports are excellent between- and within-reliability and responsiveness to change suggested that the BBS is suitable for this function.
To conclude, the addition of Tetrax program did not prove to be overall beneficial in improving balance. However, Tetrax did demonstrate benefit in specific positions.
LIMITATIONS OF THE STUDY
a) Small sample size, b) A particular type of stroke was not taken, c) Short duration of treatment.
FUTURE SCOPE
This study can be refined by improving the inclusion criteria such as a particular type of stroke- MCA, ACA stroke, etc. This study can be more refined by improving the inclusion criteria such as a particular type of stroke- hemorrhagic and ischemic stroke. The sample size can be increased. Gender differences can be checked with the effect of tetrax on standing balance.
CONCLUSION
The present study concluded a significant difference in improving balance in both the groups- group receiving only conventional therapy and group receiving the combination of tetrax and conventional therapy. However, there is no significant difference between the groups.

REFERENCES
- Truelsen T, Begg S, Mathers C. The global burden of cerebrovascular. InWho Int 2006.
- Kwakkel G, van Peppen R, Wagenaar RC, Wood Dauphinee S, Richards C, Ashburn A, Miller K, Lincoln N, Partridge C, Wellwood I, Langhorne P. Effects of augmented exercise therapy time after stroke: a meta-analysis. Stroke. 2004 Nov;35(11):2529-39. https://doi.org/10.1161/01.STR.0000143153.76460.7d. Epub 2004 Oct 7. PMID: 15472114.
- Ada L, Dorsch S, Canning CG. Strengthening interventions increase strength and improve activity after stroke: a systematic review. Aust J Physiother. 2006;52(4):241-8. https://doi.org/10.1016/s0004-9514(06)70003-4. PMID: 17132118.
- Pandian JD, Sudhan P. Stroke epidemiology and stroke care services in India. J Stroke. 2013 Sep;15(3):128-34. https://doi.org/10.5853/jos.2013.15.3.128. Epub 2013 Sep 27. PMID: 24396806; PMCID: PMC3859004.
- Prabhakar P, De T, Nagaraja D, Christopher R. Angiotensin-converting enzyme gene insertion/deletion polymorphism and small vessel cerebral stroke in Indian population. Int J Vasc Med. 2014;2014:305309. https://doi.org/10.1155/2014/305309. Epub 2014 Jan 12. PMID: 24523965; PMCID: PMC3913494.
- Kisialiou A, Grella R, Carrizzo A, Pelone G, Bartolo M, Zucchella C, Rozza F, Grillea G, Colonnese C, Formisano L, Lembo M. Risk factors and acute ischemic stroke subtypes. J Neurol Sci. 2014 Apr 15;339(1-2):41-6.
- Yamato TP, Pompeu JE, Pompeu SM, Hassett L. Virtual Reality for Stroke Rehabilitation. Phys Ther. 2016 Oct;96(10):1508-1513. https://doi.org/10.2522/ptj.20150539. Epub 2016 Apr 14. PMID: 27081204.
- Alessandra Narciso Garcia, Ana Beatriz Carvalho, Giordano Marcio Gatinho Bonuzzi, Gisele Carla de Palma, Fabio Navarro Cyrillo, Mirna Migliacci Forte Vieira, Sandra Regina Alouche, Jose Eduardo Pompeu and Camila Torriani-Pasin. Effects of using virtual reality in balance and mobility of post stroke individuals: A pilot study. Arch Med, 2015; 7(65), 01-06.
- de Oliveira CB, de Medeiros IR, Frota NA, Greters ME, Conforto AB. Balance control in hemiparetic stroke patients: main tools for evaluation. J Rehabil Res Dev. 2008;45(8):1215-26. PMID: 19235121.
- Teixeira-Salmela LF, Olney SJ, Nadeau S, Brouwer B. Muscle strengthening and physical conditioning to reduce impairment and disability in chronic stroke survivors. Arch Phys Med Rehabil. 1999 Oct;80(10):1211-8. https://doi.org/10.1016/s0003-9993(99)90018-7. PMID: 10527076.
- O’Donnell M, Xavier D, Diener C, Sacco R, Lisheng L, Zhang H, Pias P, Truelsen T, Chin SL, Rangarajan S, Devilliers L, Damasceno A, Mondo C, Lanas F, Avezum A, Diaz R, Varigos J, Hankey G, Teal P, Kapral M, Ryglewicz D, Czlonkowska A, Skowronska M, Lopez-Jaramillo P, Dans T, Langhorne P, Yusuf S; INTERSTROKE investigators. Rationale and design of INTERSTROKE: a global case-control study of risk factors for stroke. Neuroepidemiology. 2010;35(1):36-44. https://doi.org/10.1159/000306058. Epub 2010 Apr 8. PMID: 20389123.
- Dromerick AW, Lum PS, Hidler J. Activity-based therapies. NeuroRx. 2006 Oct;3(4):428-38. https://doi.org/ 10.1016/j.nurx.2006.07.004. PMID: 17012056; PMCID: PMC3593413.
- Couture M, Desrosiers J, Leclerc G. Self-actualization and poststroke rehabilitation. Int J Rehabil Res. 2007 Jun;30(2):111-7. https://doi.org/10.1097/MRR.0b013e32813a2ea5. PMID: 17473622.
- Hill K, Ellis P, Bernhardt J, Maggs P, Hull S. Balance and mobility outcomes for stroke patients: a comprehensive audit. Aust J Physiother. 1997;43(3):173-180. https://doi.org/10.1016/s0004-9514(14)60408-6. PMID: 11676685.
- Cabanas-Valdés R, Cuchi GU, Bagur-Calafat C. Trunk training exercises approaches for improving trunk performance and functional sitting balance in patients with stroke: a systematic review. NeuroRehabilitation. 2013;33(4):575-92. https://doi.org/10.3233/NRE-130996. PMID: 24018373.
- Nichols DS. Balance retraining after stroke using force platform biofeedback. Phys Ther. 1997 May;77(5):553-8. https://doi.org/10.1093/ptj/77.5.553. PMID: 9149764.
- Chen IC, Cheng PT, Chen CL, Chen SC, Chung CY, Yeh TH. Effects of balance training on hemiplegic stroke patients. Chang Gung Med J. 2002 Sep;25(9):583-90. PMID: 12479619.
- Hung JW, Yu MY, Chang KC, Lee HC, Hsieh YW, Chen PC. Feasibility of Using Tetrax Biofeedback Video Games for Balance Training in Patients With Chronic Hemiplegic Stroke. PM R. 2016 Oct;8(10):962-970. https://doi.org/ 10.1016/j.pmrj.2016.02.009. Epub 2016 Mar 9. PMID: 26968609.
- Walker C, Brouwer BJ, Culham EG. Use of visual feedback in retraining balance following acute stroke. Phys Ther. 2000 Sep;80(9):886-95. PMID: 10960936.
- Takeuchi N, Izumi S. Rehabilitation with poststroke motor recovery: a review with a focus on neural plasticity. Stroke Res Treat. 2013;2013:128641. https://doi.org/10.1155/2013/128641. Epub 2013 Apr 30. PMID: 23738231; PMCID: PMC3659508.
- http://www.sunlightnet.com/international/html/producttetrax.html
- Song YB, Chun MH, Kim W, Lee SJ, Yi JH, Park DH. The effect of virtual reality and tetra-ataxiometric posturography programs on stroke patients with impaired standing balance. Ann Rehabil Med. 2014 Apr;38(2):160-6. https://doi.org/10.5535/arm.2014.38.2.160. Epub 2014 Apr 29. PMID: 24855609; PMCID: PMC4026601.
- van Nes IJ, Nienhuis B, Latour H, Geurts AC. Posturographic assessment of sitting balance recovery in the subacute phase of stroke. Gait Posture. 2008 Oct;28(3):507-12. https://doi.org/10.1016/j.gaitpost.2008.03.004. PMID: 18424149.
ARTICLE TYPE: Research Article;
ORCID ID: Open Researcher and Contributor Identifier (ORCID) ID of corresponding author: https://orcid.org/0000-0002-8554-2516;
ETHICAL: Institutional Ethics Committee;
ACKNOWLEDGEMENT: The authors are greatful to I.T.S Institute of Health and Allied Sciences, Muradnagar, Ghaziabad and VIMHANS Niyati Super Speciality Hospital, Lajpat Nagar, New Delhi for providing us with the Tetrax apparatus and also permitting us to conduct research in their premises.;
FINANCIAL DISCLOSURE: The authors declare that there was no financial aid received.;
CONFLICT OF INTEREST: No conflict of interest associated with this research work.;
AUTHORS CONTRIBUTION: Idea and Conceptualization: Dr Bhawna Sharma and Dr Prateek Gaur, Data Collection: Dr Bhawna Sharma, Final Editing: Dr Poonam Kandian and Dr Bhawna Sharma.;
CORRESPONDING AUTHOR AFFILIATIONS: Dr. Bhawna Sharma, ITS Institute of Health and Allied Sciences, Muradnagar, Uttar Pradesh 201206, India.;
CORRESPONDING AUTHOR EMAIL: [email protected];
ARTICLE CITATION: Sharma B, Gaur P, Kadian P. Effect of tetraataxiometric posturography programs (TETRAX) on stroke patients with impaired standing balance. SALT J Sci Res Healthc. 2022 February 13; 2(1): 20-30.
PUBLISHER’S NOTE: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.




© Bhawna Sharma, Prateek Gaur, Poonam Kadian
Originally published in the SALT Journal of Scientific Research in Healthcare (https://saltjsrh.in/), 13.02.2022.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by-nc-nd/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work, first published in the SALT Journal of Scientific Research in Healthcare (https://saltjsrh.in/), is properly cited. The complete bibliographic information, a link to the original publication on https://saltjsrh.in/, as well as this copyright and license information must be included.
