PHYSIOTHERAPY REHABILITATION IN CHRONIC KIDNEY DISEASE ALONG WITH CARDIOVASUCLAR COMPLICATIONS – CASE STUDY IN ICU SETTINGS
SALT Journal of Scientific Research in Healthcare
Volume 2, Issue 2, Page 30-34, Published on 30th December 2022
https://doi.org/10.56735/saltjsrh.ms2202023034
Case Report
PHYSIOTHERAPY REHABILITATION IN CHRONIC KIDNEY DISEASE ALONG WITH CARDIOVASUCLAR COMPLICATIONS – CASE STUDY IN ICU SETTINGS
MANISH KUMAR AND SHILPA GUPTA
Department of Physiotherapy, Sharda University, Greater Noida 201306 , India
Corresponding Author: Mr. Manish Kumar, Intern, Department of Physiotherapy, Sharda University, Greater Noida 201306, India.
ORCID ID: 0000-0002-5322-9066
ABSTRACT
Chronic kidney disease or kidney damage leads to decline in glomerular filtration rate (GFR) that lasts for three months or more. Chronic kidney disease (CKD) and heart failure (HF) coexist, and it’s thought that roughly 50% of HF patients also have CKD. The following case study is done to interpret the effects of physiotherapy on CKD patient in ICU setting. The goal of the treatment was to decrease shortness of breathing, to maintain the patency of the lungs, to remove the secretions, to maintain the secondary complications and to do early mobilization to make patient independent in ADLs. Outcome measures used were The Timed Up and Go (TUG), Borg rating of perceived exertion (RPE) and SF-36. Along with the improvement of QOL, patient reported Lower levels of discomfort and improved rest and sleep patterns after physiotherapy interventions.
Keywords: Chronic kidney disease, physiotherapy in ICU, chest physiotherapy
INTRODUCTION
Chronic kidney disease or kidney damage leads to decline in glomerular filtration rate (GFR) that lasts for three months or more. Additionally, the global CKD is becoming a serious public health issue resulting in low quality of life and poor self-management.1 According to estimates, more than 1 in 7, or 15% of US adults, or 37 million persons are having CKD.2 Acute kidney injury (AKI), CKD are now estimated to affect more than 850 million people globally, according to the International Society of Nephrology [ISN],(2020).3 Patients with CKD are at significant risk for cardiovascular disease, which is the main cause of death.4 Increased albuminuria and low GFR are linked to an increased risk of Cardio Vascular Diseases.5 CKD is a factor that leads to low Ejection fraction in patients and increases the risk of heart failure.6 Chronic kidney disease (CKD) and heart failure (HF) coexist, and it’s thought that roughly 50% of HF patients also have CKD.7
People with advanced chronic renal disease require immediate care in order to maintain their lives, one of them is Hemodialysis is used.8 Hemodialysis is a medical procedure that restores kidney function by having the patient’s blood circulate through a dialyzer tube outside of their body.9
Percussion, vibration, suctioning, respiratory muscle strengthening, breathing exercises, mobilization, Positioning, manual and ventilator hyperinflation, non-invasive ventilation, weaning from mechanical ventilation and education, are some of the interventions that may be used in respiratory physiotherapy.10 Those who survive protracted ICU stays spend a lot of time in bed and are immobile. In order to get ongoing medical attention and rehabilitation, these patients are frequently transferred to long-term acute care hospitals (LTACHs). Early ambulation is linked to with better functional results and fewer hospitalization patients returning for readmission.11 Early mobilisation, during the first few days of admission to a medical ICU, improves outcomes, functionality, and self-care after discharge while reducing length of stay and death. incentive spirometry with Deep breathing exercises use the patient’s diaphragm to create negative pressure, rather than the accessory respiratory muscles, to move air into the lungs. This can improve lung recruitment and oxygenation, raise functional residual capacity and tidal volume, and possibly aid in secretion clearance.13
The Timed Up and Go (TUG) test is an easy mobility evaluation that calls for both static and dynamic balance.14 Borg rating of perceived exertion (RPE) is a scale used to determine the recommended exercise intensity. In cardiac patients as well as other patient populations undertaking rehabilitation and endurance training, it is utilized to assess exercise progress and mode.15
The SF-36 is made to evaluate health concepts in adults that are pertinent to all age, disease, and treatment groups.16 Created in the early 1990s and consisting of 36 questions, is a questionnaire that covers all facets of health. Normal values for individuals of working age are available, and it has been used in a variety of settings, including primary care. It includes questions that are grouped into eight categories and ask about functional status, emotional and social well-being, and general health evaluation (or dimensions). with ratings ranging from 0 to 100 for each of these scales (or dimensions). Higher scores correspond to better HRQoL. The range of the SF-36 is 0 (worst) to 100 (best). The SF-36 may be a valuable instrument for gauging outcomes after critical illness due to its general nature, history of usage outside of intensive care, and accessibility to normal data.17,18
PATIENT DESCRIPTION
A 65-year-old male patient from Greater Noida, diagnosed with CKD from past 5 years, decompressed myopathy, and coronary artery disease, was admitted to Sharda Hospital on 8th September 2022, with the complaint of dyspnea at rest which was progressive in nature along with restlessness. The patient was a businessman by profession and had a history of occasional drinking and chronic smoking. On receiving the patient to the emergency department (EW), he had an episode of cardiopulmonary arrest and was revived through CPR. Following intubation, the patient was placed on ventilator assistance (A/C VC mode) with a Fio2 of 40% and a PEEP of 6. Thereafter the patient was moved from EW to ICU. Patient was kept on Mechanical Ventilator (MV) for four days before being extubated, after which required four liters of additional oxygen to maintain 100% Spo2. Every third day, hemodialysis was also being performed on the patient, who had already had three sessions.
The patient had hypotension. On an average the patient was having 100/70mmHg blood pressure. The Ejection Fraction of the patient on average for period of 10 days was 22.5%.
The ABG reading of the patient were metabolic acidosis in the beginning for 2 days then become respiratory acidosis on 3rd day after that from day 4 till day 9 it was metabolic acidosis then on 10th day it become respiratory acidosis these changes may be due to drug therapy and hemodialysis (refer to Table 1).
Outcome measures
The outcome measures used in this study are (i) The Timed Up and Go (TUG) test, (ii) Borg rating of perceived exertion (RPE), and (iii) SF-36.
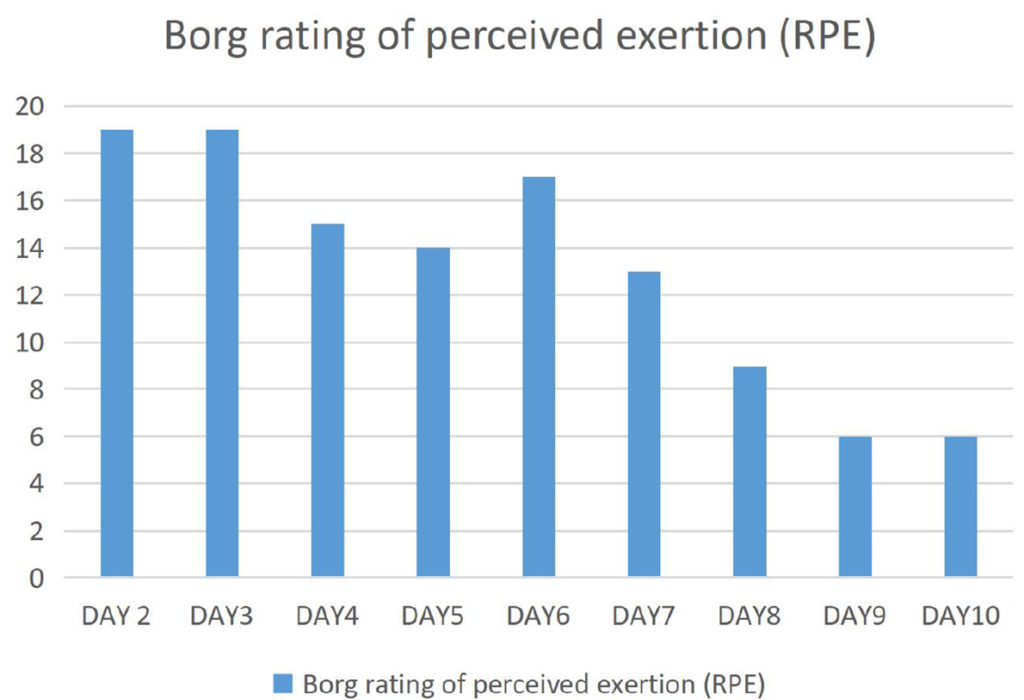
After intervention, the outcome measurements were gathered. The Borg rating of perceived exertion (RPE) was recorded every day from day 2 of the ICU treatment to day 10 (Figure 1).
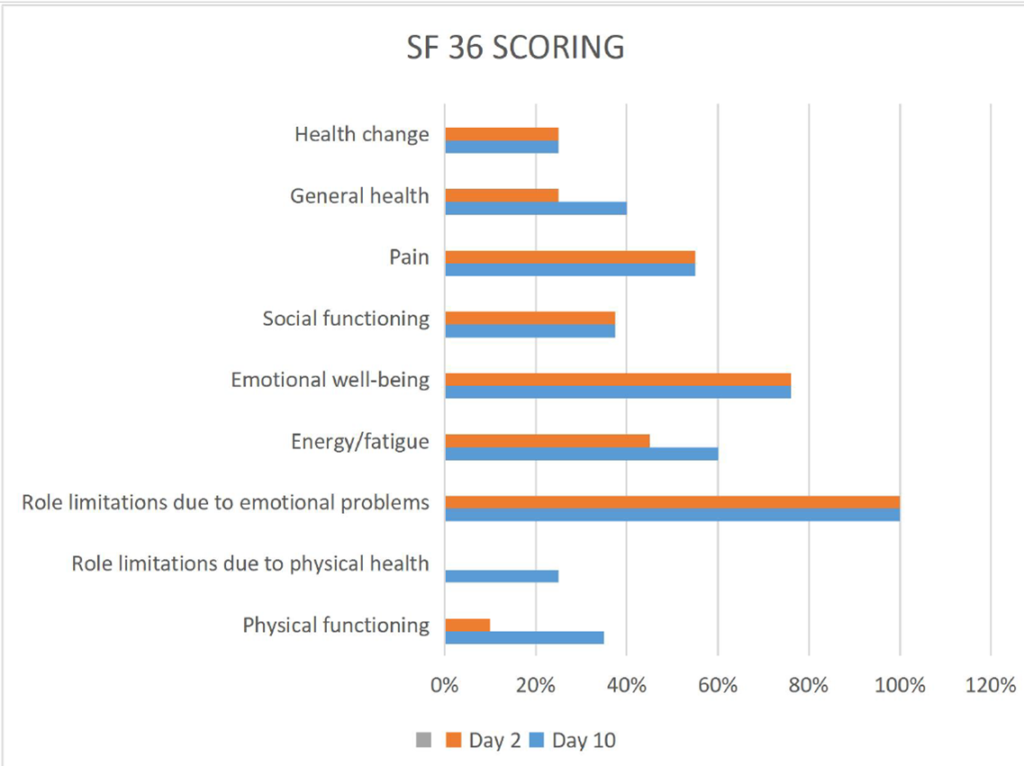
On days 2 and 10 of the treatment, SF 36 scoring was performed to assess the efficacy (Figure 2). On day 10, a time-up-and-go test was conducted.
Treatment
The goal of the treatment was to decrease shortness of breathing, to maintain the patency of the lungs, to remove the secretions, to maintain the secondary complications and to do early mobilization to make patient independent in ADLs.
Day 1- (Patient was on supplemental oxygen 4 lt) treatment start post extubation on day 4 of admission to ICU. Post extubation percussion and vibrations were given posteriorly after that nebulization was given for 15 mins. After one hour incentive spirometry (5 sets of 10 reps), vol 600cc in gravity eliminated position. Spo2 97%.
Day 2- (Patient was on supplemental oxygen 4lt), incentive spirometry (5sets of 10 reps) vol 600cc against gravity, deep breathing exercises with 5 sec hold, percussion, vibrations, forceful expiratory techniques (huffing and coughing) and high sitting with minimal support. And active assisted range of motion exercises for both upper limb and lower limb. Spo2 98%.
Borg rating of perceived exertion (RPE) was explained to the patient and asked about the scoring. Borg rating of perceived exertion (RPE)-19.
| Physical functioning | 10% |
| Role limitations due to physical health | 0% |
| Role limitations due to emotional problems | 100% |
| Energy/fatigue | 45% |
| Emotional well-being | 76% |
| Social functioning | 37.5% |
| Pain | 55% |
| General health | 25% |
| Health change | 25% |
Day 3-(Patient was on supplemental oxygen 2lt) incentive spirometry (5sets of 10 reps) vol 900cc against gravity, out of bed mobilization and rest of the same treatment as day 2. And active range of motion exercises for both upper and lower limb. Spo2 98%.
Borg rating of perceived exertion (RPE)- 19.
Day 4-(Patient was on supplemental oxygen 4lt and during ambulation increased to 6lt with portable cylinder) ambulation 10 steps after that patient feel dizziness, rest treatment same as day 3. Spo2 100%.
Borg rating of perceived exertion (RPE)- 15.
Day 5-(Patient was on supplemental oxygen 4lt and during ambulation increased to 6lt with portable cylinder) ambulation 200m for around 15 minutes, rest treatment same as day 3. Spo2 100%.
Borg rating of perceived exertion (RPE)- 14.
Day -6 patient was again put on non-invasive ventilator after fall in SPO2 77% during Hemodialysis.
Patient was kept of NIV over night at first, the NIV for 2 hours in day after that supplemental oxygen 4lt in for next 4 hours. Spirometry, percussion vibration and bed side high sitting was continued.
Borg rating of perceived exertion (RPE)- 17.
Day 7-(Patient was on supplemental oxygen 4lt and during ambulation increased to 6lt with portable cylinder) same treatment as day 5 was followed adding ambulation for 300m. Spo2 100% decreased to 98% during ambulation.
Borg rating of perceived exertion (RPE)- 13.
Day 8-(Patient was on supplemental oxygen 2 liters and during ambulation increased to 4lt with portable cylinder) same treatment as day 5 was followed adding ambulation for 400m. SpO2 100%.
Borg rating of perceived exertion (RPE)- 9.
Day 9-(Patient was on supplemental oxygen 2lt and during ambulation increased to 4lt with portable cylinder) same treatment as day 7 patient was ambulated for 500 m without any exertion.
Borg rating of perceived exertion (RPE)- 6.
Day 10- on day 10 time up and go test was performed. Firstly, test was explained to the patient.
It took 12 seconds for patient to complete the test. Which was quite good.
Borg rating of perceived exertion (RPE)- 6.
| Physical functioning | 35% |
| Role limitations due to physical health | 25% |
| Role limitations due to emotional problems | 100% |
| Energy/fatigue | 60% |
| Emotional well-being | 76% |
| Social functioning | 37.5% |
| Pain | 55% |
| General health | 40% |
| Health change | 25% |
| Date | ABG Interpretation |
| 08.09.22 | Metabolic acidosis |
| 09.09.22 | Metabolic acidosis |
| 10.09.22 | Respiratory acidosis (fully compensated) |
| 11.09.22 | Metabolic acidosis(partially compensated) |
| 12.09.22 | Metabolic acidosis(uncompensated) |
| 13.09.22 | Metabolic acidosis(uncompensated) |
| 14.09.22 | Metabolic acidosis |
| 15.09.22 | Metabolic acidosis(uncompensated) |
| 17.09.22 | Metabolic acidosis(partially compensated) |
| 18.09.22 | Respiratory acidosis (uncompensated) |
| 19.09.22 | Respiratory acidosis (partially compensated) |
| 20.09.22 | Respiratory acidosis (partially compensated) |
| 21.09.22 | Fully Compensated Respiratory acidosis |
DISCUSSION
CKD is linked with cardiovascular diseases, decreased endurance, quality of life, dependency, low ejection fraction leading to cardiac arrest and even death. Patient with CKD are prone to be critically ill and may require Intensive Care. Also, with progression in disease patient will become hemodialysis dependent. Improvements in HR and SBP response as well as a reduced need for additional oxygen during exercise are among the main physiologic and functional changes seen in this case study.
The quality of life and physical capabilities of chronic kidney disease patients could significantly improve with the implementation of a physiotherapy programme during hemodialysis.19 Patients with CKD demonstrate an improvement in their overall QOL during hemodialysis, which encourages the inclusion of a physiotherapy programme in their everyday lives for positive and consistent changes in their quality of life. As Reported by Lara et al., One of the benefits of practising exercise is related to the enhancement of cardiovascular parameters, improvement of quality of life, and survival in both the general population and the population of patients with chronic conditions.20 which was similar to results as seen in our case study. Along with the improvement of QOL, patient reported Lower levels of discomfort and improved rest and sleep patterns after physiotherapy interventions. These changes may result in better cardiovascular health, a lower level of oxygen dependency, a reduction in the need for painkillers, and less fatigue and sleepiness. Other effects include increased willingness to carry out daily tasks and, an improvement in selfesteem and body image, which is followed by an increased socializing. With reference to hypotension there were not such changes seen. According to Soares et al.,21 there are two types of arterial hypotension: the first one typically occurs at the end of treatment, and the other, which is a chronic and persistent form, occurs in a group of patients who have systolic blood pressure that was lower than 90-100 mmHg before beginning dialysis and whose frequency decreases more as the dialysis progresses. One of the causes of hypotension is linked to cardiac variables, such as a cardiac deficit that is too dependent on diastolic dysfunction, an inability to increase heart frequency, or usage of beta blockers, uremic neuropathy, or ageing, among other things.
CONCLUSION
This study concludes that early mobilization and ambulation along with other techniques of cardiopulmonary rehabilitation are effective in improving ABG values, QOL and decreasing dependency on supplemental Oxygen in CKD patients with history of an episode of cardiac arrest along with other cardiopulmonary complications.
REFERENCES
- Kumar Dasari B, Manishkumar T, Anchuri S, Vallepu N, Adepu P. A case report on Chronic Kidney Disease and Role of Clinical Pharmacist. PharmaTutor. 2019 Jan 1;7(1):59-62. https://doi.org/10.29161/PT.v7.i1.2019.59.
- Hargrove N, Tays Q, Storsley L, Komenda P, Rigatto C, Ferguson T, Tangri N, Bohm C. Effect of an exercise rehabilitation program on physical function over 1 year in chronic kidney disease: an observational study. Clin Kidney J. 2019 Apr 21;13(1):95-104. https://doi.org/10.1093/ckj/sfz037. PMID: 32082557; PMCID: PMC7025337.
- CDC. Chronic Kidney Disease in the United States, 2019 fact sheet. CDC. 2019;1(2):1-6.
- ISN. The International Society of Nephrology ( ISN ). Int Soc Nephrol. Published online 2020:3-5.
- Jankowski J, Floege J, Fliser D, Böhm M, Marx N. Cardiovascular Disease in Chronic Kidney Disease: Pathophysiological Insights and Therapeutic Options. Circulation. 2021 Mar 16;143(11):1157-1172. https://doi.org/10.1161/CIRCULATIONAHA.120.050686. Epub 2021 Mar 15. PMID: 33720773; PMCID: PMC7969169.
- Chronic Kidney Disease Prognosis Consortium; Matsushita K, van der Velde M, Astor BC, Woodward M, Levey AS, de Jong PE, Coresh J, Gansevoort RT. Association of estimated glomerular filtration rate and albuminuria with all-cause and cardiovascular mortality in general population cohorts: a collaborative meta-analysis. Lancet. 2010 Jun 12;375(9731):2073-81. https://doi.org/10.1016/S0140-6736(10)60674-5. Epub 2010 May 17. PMID: 20483451; PMCID: PMC3993088.
- Mavrakanas TA, Khattak A, Wang W, Singh K, Charytan DM. Association of Chronic Kidney Disease with Preserved Ejection Fraction Heart Failure Is Independent of Baseline Cardiac Function. Kidney Blood Press Res. 2019;44(5):1247-1258. https://doi.org/10.1159/000502874. Epub 2019 Sep 2. PMID: 31476759.
- van de Wouw J, Broekhuizen M, Sorop O, Joles JA, Verhaar MC, Duncker DJ, Danser AHJ, Merkus D. Chronic Kidney Disease as a Risk Factor for Heart Failure With Preserved Ejection Fraction: A Focus on Microcirculatory Factors and Therapeutic Targets. Front Physiol. 2019 Sep 4;10:1108. https://doi.org/10.3389/fphys.2019.01108. PMID: 31551803; PMCID: PMC6737277.
- Rahayu F, Fernandoz T, Ramlis R. Hubungan frekuensi hemodialisis dengan tingkat stres pada pasien gagal ginjal kronik yang menjalani hemodialisis. Jurnal keperawatan silampari. 2018 Mar 24;1(2):139-53. Retrieved from: https://media.neliti.com/media/publications/256091-hubunganfrekuensi-hemodialisis-dengan-ta5e0cf49.pdf.
- Esteras R, Martín-Navarro J, Ledesma G, Fernández-Prado R, Carreño G, Cintra M, Cidraque I, Sanz I, Tarragón B, Alexandru S, Milla M, Astudillo E, Sánchez E, Mas S, Tejeiro RD, Ortiz A, Sánchez R, González-Parra E. Incidence of Hypersensitivity Reactions During Hemodialysis. Kidney Blood Press Res. 2018;43(5):1472-1478. https://doi.org/ 10.1159/000493662. Epub 2018 Sep 20. PMID: 30235456.
- Chartered Society of Physiotherapy, Physiotherapy works: critical care. Accessed on 2/6/19 http://www.csp.org.uk/publications/physiotherapyworks-critical-care.
- Tran DH, Maheshwari P, Nagaria Z, Patel HY, Verceles AC. Ambulatory Status Is Associated With Successful Discharge Home in Survivors of Critical Illness. Respir Care. 2020 Aug;65(8):1168-1173. https://doi.org/10.4187/respcare.07437. Epub 2020 Mar 31. PMID: 32234767; PMCID: PMC7538008.
- Escalon MX, Lichtenstein AH, Posner E, Spielman L, Delgado A, Kolakowsky-Hayner SA. The Effects of Early Mobilization on Patients Requiring Extended Mechanical Ventilation Across Multiple ICUs. Crit Care Explor. 2020 Jun 8;2(6):e0119. https://doi.org/10.1097/CCE.0000000000000119. PMID: 32695988; PMCID: PMC7314317.
- Pathmanathan N, Beaumont N, Gratrix A P. Respiratory physiotherapy in the critical care unit. Continuing Education in Anaesthesia, Critical Care & Pain. 2015;15: 20-5.
- “Timed Up and Go (TUG)”. Minnesota Falls Prevention. Retrieved 2010-02-16.
- Rating of perceived exertion. Available from: https://en.wikipedia.org/wiki/Rating_of_perceived_exertion(accessed 24 May 2019).
- Ware JE Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992 Jun;30(6):473-83. PMID: 1593914.
- Chrispin PS, Scotton H, Rogers J, Lloyd D, Ridley SA. Short Form 36 in the intensive care unit: assessment of acceptability, reliability and validity of the questionnaire. Anaesthesia. 1997 Jan; 52(1):15-23.
- Stolić R, Mihailović B, Matijašević IR, Jakšić MD. Effects of physiotherapy in patients treated with chronic hemodialysis. Biomedicinska istraživanja. 2018;9(1):103-11.
- Lara CR, Santos FO, de Jesus Silva T, Camelier FW. Qualidade de vida de pacientes renais crônicos submetidos à fisioterapia na hemodiálise. Ciência & Saúde. 2013 Dec 18;6(3):163-71.
- Soares KT, Viesser MV, Rzniski TA, Brum EP. Efficacy of a physical exercises protocol in patients with chronic renal failure during treatment of hemodialysis, valued by SF-36. Fisioterapia em Movimento. 2011;24:133-40.
ARTICLE TYPE: Case Report;
ORCID ID: Open Researcher and Contributor Identifier (ORCID) ID of corresponding author: https://orcid.org/0000-0002-5322-9066;
ETHICAL: Institutional ethical committee and prior patient consent obtained;
ACKNOWLEDGEMENT: None;
FINANCIAL DISCLOSURE: The authors declare that there was no financial aid received.;
CONFLICT OF INTEREST: No conflict of interest associated with this research work.;
AUTHORS CONTRIBUTION: Idea and Conceptualization: MK., Data Collection and editing: SG;
AUTHORS AFFILIATIONS: Mr. Manish Kumar, Intern, Department of Physiotherapy, Sharda University, Greater Noida 201306, India; Ms. Shilpa Gupta, Associate Professor, Department of Physiotherapy, Sharda University, Greater Noida 201306, India;
CORRESPONDING AUTHOR EMAIL: 2018009721.manish@ug.sharda.ac.in; nohwarmanish6@gmail.com;
ARTICLE CITATION: Manish Kumar and Shilpa Gupta. Physiotherapy rehabilitation in chronic kidney disease along with cardiovascular complications– case study in ICU settings. SALT J Sci Res Healthc. 2022 December 30; 2(2): 30-34.
PUBLISHER’S NOTE: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
