PHYSIOTHERAPY IN POST EXCISION AND CURETTAGE OF GIANT CELL TUMOUR–EVIDENCE BASED CASE STUDY
SALT Journal of Scientific Research in Healthcare
Volume 2, Issue 2, Page 24-29, Published on 14th November 2022
https://doi.org/10.56735/saltjsrh.ms2202022429
Case Report
SUBRAMANIAN SS , LAKSHMIPRABHA K, SHALINI RV
Sree Balaji College of Physiotherapy,
Bharath Institute of Higher Education and Research,
Chennai,Tamil Nadu, India
Corresponding Author: Dr. S.S. Subramanian, Principal and Dean, Sree Balaji College of Physiotherapy, Bharath Institute of Higher Education and Research, Chennai, India.
ORCID ID:0000-0002-9944-6250
ABSTRACT
Introduction: Incidences of oncological ailments were reported, especially at an early age; one among them includes GCT (Giant Cell Tumour), commonly recorded in adulthood, affecting the lower end of the femur, the upper end of the tibia, and the lower end of the radius. This Benign lesion can give rise to compression over Neurovascular structures, which may result in pain, swelling and interfere with joint function, while amputation for GCT was used earlier. Materials and Methods: This study where a 19-year-old Female with pain and difficulty in daily functional activities like walking, squatting, and stair activity and also with weight loss and fatigue for more than two months was diagnosed with a Giant Cell Tumour of Left lower medial femoral condyle on 23rd August 2022. She was treated with Curettage filled with Bone cement and fixed with a Locking Compression Plate on 30th August 2022. The subject was started with immediate postoperative physiotherapy and continued for up to 8 weeks. Results: The outcome measures were analysed and discussed with due evidence using a patient-specific functional scale. Conclusion: With lesser research on Onco physiotherapy, results and outcome measures of this case study get highly informative and more significant, highlighting the required role of Physiotherapy in Preventing muscle Atrophy, Joint stiffness, and Greater Functional Restoration.
Keywords: Giant cell tumour, Benign, Neurovascular, Atrophy, Bone Cancer, Quality of life
INTRODUCTION
Advancement in medical knowledge hugely necessitates the practical application of the learned material for the health benefits of affected subjects. Along with an improved standard of living and unknown clinical conditions, including Giant Cell tumours, lesser research on adolescent females is discussed with evidence here, (Ghouchani et al., 2018).
Non-traumatic cause of functional disturbances, especially of knee instability with atrophy, needs more probable clinical reasoning. Tumours are commonly seen elsewhere in the body. Giant cell tumours of the bone are benign multi-nucleated cell masses commonly found at the epiphyses and sometimes the metaphysis of long bones.
It is due to the osteoclastic function of bone cells due to gene mutation (H3F3A) H3 Histone, Family 3A (H3F3A) is a gene that encodes a histone, Wagrodzki et al., 2022; GCT is of the unknown cause having evidence of genetic origin, while Goodman, 2007 stated that common age group is 20-55 years and female are affected than male, (Valerae, 2011).
Clinical Signs: Pain, Synovitis, Decreased Rom of knee, Muscle atrophy, Weight loss, Insomnia, Fatigue, Difficulty in ADL (Activities of Daily Living), and Cognitive dysfunction (Gupta & Khadke, 2017).
Causes for Non-traumatic knee instability are so many, which includes infection like Tuberculosis, Bursitis, Osteopenia, patellar dysfunction, arthritis, nerve lesion, spinal cord tumour, cancer, benign tumour, GCT etc. Fotiadou & Karantanas, 2009.
Early intervention by medical referral could benefit greater outcomes post giant cell tumour of the femur, as evidenced by Rigollino et al., 2017. Whereas a decline in health and physical functioning even after treatment among ten synovial GCT was recorded by Mastboon et al., 2019, Contradictory to another research that shows better QOL in post-surgical GCT (Verspoor et al., 2019).
The chances of recurrence and contradictory post-surgical outcome of GCT of the femur were discussed with evidence on timely identification by physiotherapists and reasonable postoperative functional prognosis. According to AAOS 2011, post-GCT surgical excision followed by physiotherapy is explained in this research, and also widening the scope of physiotherapy in the post on surgical intervention in GCT.
AIM AND OBJECTIVES
The aim and objective of this research were
1. To analyse the early identification of GCT by Physiotherapist clinically.
2. To evaluate the post-surgical GCT physiotherapy role.
Scope and Need: The scope and need of this research were an increasing GCT early screening with learned evidenced knowledge in probable non-traumatic instability of the knee, pain, atrophy of quadriceps, and functional limitations can better be used clinically as red flags for physiotherapy as these needs’ medical intervention.
MATERIALS AND METHODOLOGY
A 19-year adult regularly menstruating female weighing 85 kgs was suddenly noted with loss of weight, antalgic gait, fatigue, and disturbances with knee functioning was referred for orthopaedic investigations, which revealed GCT and subject was treated with curettage and bone cement with Locking Compression Plate.


PROCEDURE
Postoperative physiotherapy includes from September to October 2022.
Patient care point: Long leg brace advised to wear continuously in 1 week; Toilet activity in bed side for 1 or 2 pod; NO side lying for a 1 week; NWB gait with walker support; CPM as much as pain tolerated.

Other exercises as follows:
Other exercises are as follows:
1 POD (Post Operative Day):
Breathing exercises, Ankle pump exercises 5 rep/hour, Isometrics for quadriceps and Hamstrings, Unilateral Pelvic bridging exercises, Contralateral limb maintenance exercises twice a day, Upper limb mobilisation and strengthening exercises twice a day, CPM (Continuous Passive Motion) 0-30/30 min/once a day.
2 POD to 7 POD: Same as 1 POD and NWB (Non Weight Bearing) gait training, Toilet activity encouraged in western toilet, Isometric abdominals, CPM angle increased with pain tolerance, Gradual knee mobilisation in high sitting tolerated by the patients pain perception.
From 8th day: Patient was discharged with the home plan, active knee mobilisation exercises in high sitting, active hip mobilisation, upper limb and contralateral limb maintenance and strengthening exercises, core exercise, ankle mobilisation, knee active mobilisation, isometrics for quadriceps, vastus medialis, Hamstrings, NWB gait training; 15th-day sutures removed. The patient continued with all exercises for up to 6 weeks.
7th week to 16th week:
Check X-ray taken; after that, patient was encouraged to walk without a brace, side-lying encouraged, Prone lying knee bending exercise, Toe touch gait initiated and slowly encouraged to weight bear as much pain tolerated.
RESULTS
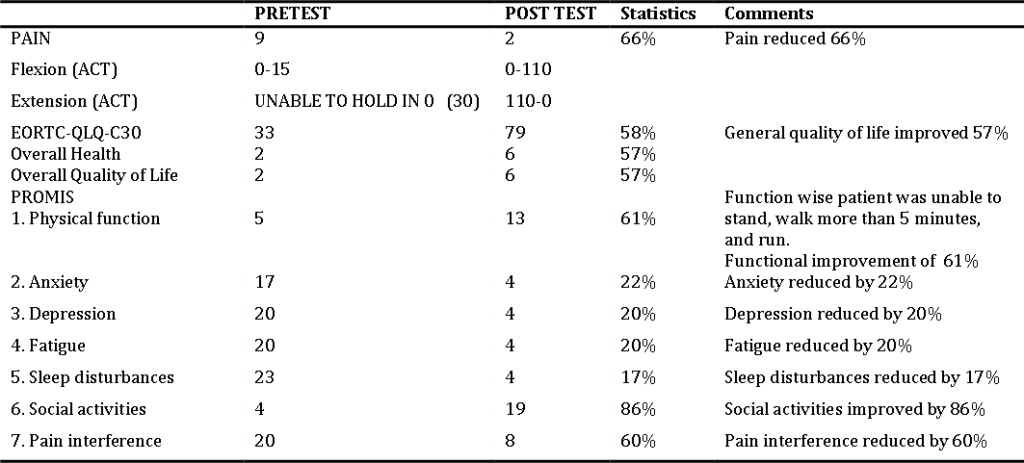
1. Outcome measure was taken for pain, using NPRS (Numerical Pain Rating Scale) in the left knee.
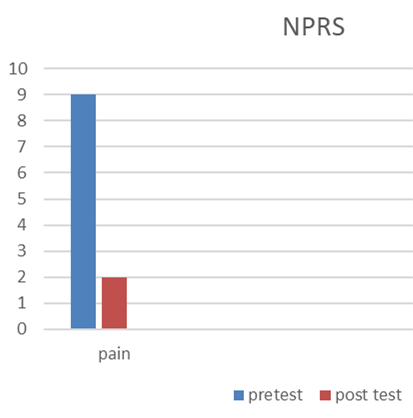
2. ROM (Range of Motion) of left Knee
3. EORTC-QLQ-C30 (European Organisation of Research and Treatment in Cancer- Quality of Life Questionnaire).
4. PROMIS-29 (Patient Reported Outcomes Measurement Information System)
Table 1 : Results of pre and post NPRS, ROM of knee, EORTC-QLQ-C30, PROMIS-29
DATA ANALYSIS
NPRS: The subject was assessed for pain, range of motion of the left knee joint, and quality of life and pre and post-data was compared.
Pain experienced by the patient before surgery was un-tolerable and unbearable, preventing the daily activities. After excision, the pain felt by patient was only incisional pain and also subject was able to do her ADL without pain.
ROM: Pre–operatively, knee movements were unable to do by the subject actively due to pain, but the passive range was there in the left knee. Eight weeks after surgery, the knee flexion was improved and also extension. She was able to lock her knee during gait. And she was able to hold in 0 extensions for a while, like 5 to 10 seconds. But she was able to hold in 100 extensions for 3 minutes and above.
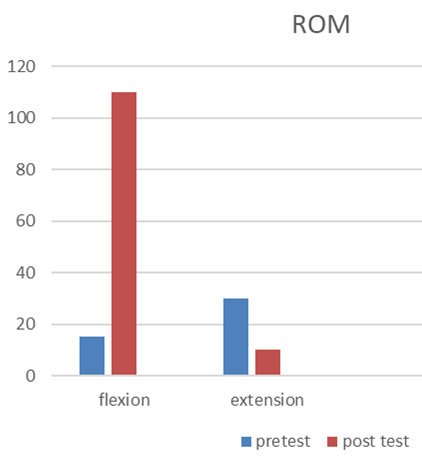
EORTC-QLQ-C30
The EORTC Core quality of life questionnaire is formatted to evaluate cancer patients’ physical, psychological and social functions. This questionnaire is filled with complex and simple questions. This is calculated as a total score, and a high score indicates better HRQOL.
Graph 3: Pre and Post EORTC-QLQ-C30
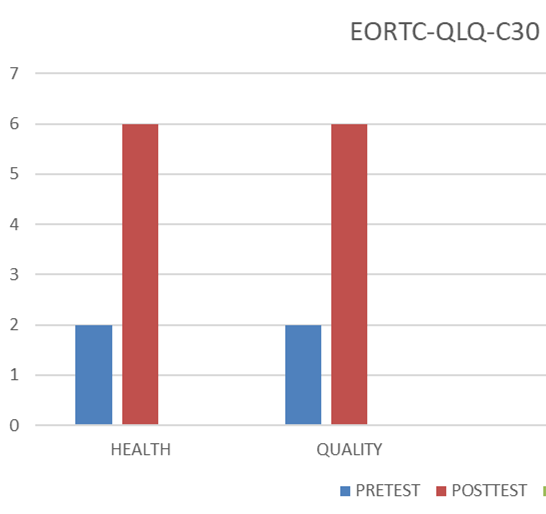
PROMIS 29
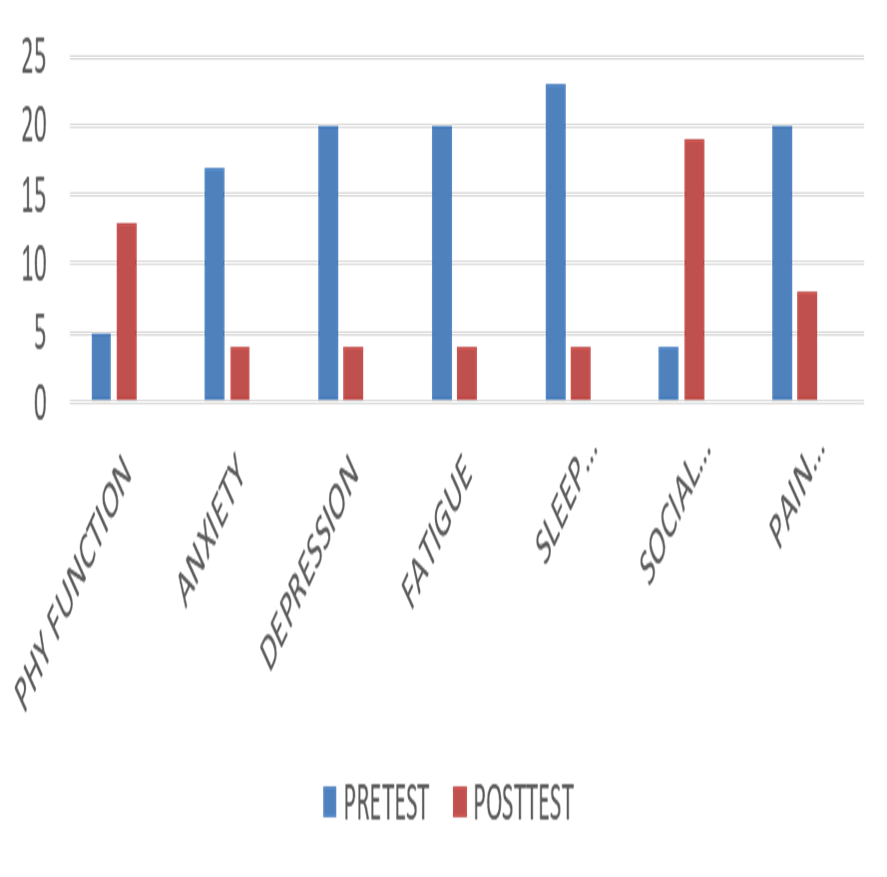
Graph 4: Pre and post PROMIS 29
PROMIS 29
PROMIS 29 TOOL was developed to assess the non-specific measure of patient scale-related health and function. The tools assessed were physical function, anxiety, and depression. Fatigue, sleep, social activities, and pain. Pre and post score showed a drastic change and improvement in cognitive function too.
Discussion
Oda et al., 1998 highlighted the importance of long-term functional follow-up for GCT, as recurrence was reported similarly, this research was into eight weeks good functional recovery was achieved, as shown in the table of results, but patient’s physiotherapy follow-up was to be continued.
Gillespie et al., 2011 reported the gender issues and proved females are more affected than males. In the research also, the subject was a 19-year adolescent female. This gender difference was again recorded by Hu Y et al., 2016.
In a 15-year follow-up from 1995 to 2009 post-CG surgically treated subjects, 34% were from the femoral origin as this subject had a femoral lesion. A clinically good prognosis was noted with no complications.
Hannah et al., 2016 recorded GCT off the distal femur of 24-year-old women treated surgically and followed by physiotherapy in 16 weeks of therapy. In contrast, this research was conducted eight weeks postoperatively GCT was reported with a reasonable prognosis, as shown in the table of results, and was working scientifically.
An Italian study of a 16-year-old GCT with a genetic history suggestive of surgical intervention and bone grafting followed by regular physiotherapy for functional restoration, including strength mobility and stability of the affected knee joint as recorded by Ambrosi et al., 2021 similar to this research subject’s genetic history, course of GCT and postoperative physiotherapy were worthy stating here.
As GCT treated surgically can influence biomechanical risk disturbances with changes in mechanical load distributions can cause adverse reactions on other peripheral joints as reported by Traub et al., 2013, exercises were provided to hip foot spine, and contralateral leg further progression to osteoarthritis were reported by Suzuki et al., 2007. However, it is early, with eight weeks of postoperative physiotherapy; this subject needs further therapy and follow-up to conclude other pathological changes in this subject.
Verspoor et al., 2019 recorded 359 GCT subjects in a five-year follow-up with greater HRQOL (Health-Related Quality of Life), similar to the findings of this study subject with good HRQOL as displayed in the table of results.
As compared to past treatment as therapy for GCT, including amputations wide resection, this subject who was treated using curettage and bone cement with ICP has shown so far no complications with good functional recovery and supported by Hosseinzadeh et al., 2022.
CONCLUSION
Early identification of Non Traumatic knee instability due to GCT should be considered among multiple aetiologies by the clinician. Timely medical intervention can lead to greater functional recovery for the affected female subject, as evidenced by this research. However, being a single case experimental design, a known limitation of this research, but continuous follow-up with physiotherapy of the study subject makes open for further scientific inferences remaining a pillar of strength of this study.
REFERENCES
- Ghouchani A, Ebrahimzadeh MH, Rouhi G. The Most Appropriate Reconstruction Method Following Giant Cell Tumor Curettage: A Biomechanical Approach. Arch Bone Jt Surg. 2018 Mar; 6(2): 85-89. PMID: 29600259; PMCID: PMC5867362.
- Wągrodzki M, Tysarowski A, Seliga K, Wojnowska A, Stepaniuk M, Castañeda Wysocka P, Makuła D, Pieńkowski A, Szostakowski B, Zub R, Rutkowski P. Diagnostic Utility of Genetic and Immunohistochemical H3-3A Mutation Analysis in Giant Cell Tumour of Bone. International Journal of Molecular Sciences. 2022; 23(2):969. https://doi.org/10.3390/ijms23020969.
- Goodman CC and Snyder TK. Differential Diagnosis for Physical Therapists: Screening for Referral. 4th edition. St. Louis, Missouri: Saunders Elsevier, 2007.
- Valerae LO. eMedicine from WebMD. Giant Cell Tumor. http://emedicine.medscape.com/article/1255364-overview. Updated April 02, 2009. Accessed March 05, 2011.
- Gupta AK, Khadke P. Cancer pathology: panel of diagnostic markers for cancer. Current Science. 2017 May 10:1831-8.
- Fotiadou A, Karantanas A. Acute nontraumatic adult knee pain: the role of MR imaging. Radiol Med. 2009 Apr;114(3):437-47. https://doi.org/10.1007/s11547-009-0380-z. Epub 2009 Apr 14. PMID: 19444384.
- Rigollino AV, Fernando TS, Tanaka MH, Souza MM. Giant cell tumor locally advanced around the knee: treatment and literature review. Rev Bras Ortop. 2017 Jun 27;52(4):473-478. https://doi.org/10.1016/j.rboe.2017.06.009. PMID: 28884107; PMCID: PMC5582821.
- Mastboom MJL, Staals EL, Verspoor FGM, Rueten-Budde AJ, Stacchiotti S, Palmerini E, Schaap GR, Jutte PC, Aston W, Leithner A, Dammerer D, Takeuchi A, Thio Q, Niu X, Wunder JS, van de Sande MAJ; Tenosynovial Giant Cell Tumors (TGCT) Study Group. Surgical Treatment of Localized-Type Tenosynovial Giant Cell Tumors of Large Joints: A Study Based on a Multicenter-Pooled Database of 31 International Sarcoma Centers. J Bone Joint Surg Am. 2019 Jul 17;101(14):1309-1318. https://doi.org/10.2106/JBJS.18.01147. Erratum in: J Bone Joint Surg Am. 2020 May 20;102(10):e49. PMID: 31318811.
- Verspoor FGM, Mastboom MJL, Hannink G, Maki RG, Wagner A, Bompas E, Desai J, Italiano A, Seddon BM, van der Graaf WTA, Blay JY, Brahmi M, Eberst L, Stacchiotti S, Mir O, van de Sande MAJ, Gelderblom H, Cassier PA. Long-term efficacy of imatinib mesylate in patients with advanced Tenosynovial Giant Cell Tumor. Sci Rep. 2019 Oct 10;9(1):14551. https://doi.org/10.1038/s41598-019-51211-y. PMID: 31601938; PMCID: PMC 6786996.
- The American Academy of Orthopaedic Surgeons. Giant Cell Tumor of Bone. http://orthoinfo.aaos.org/topic.cfm?topic=a00080. Updated June 2010.and March 05, 2011.
- Oda Y, Miura H, Tsuneyoshi M, Iwamoto Y. Giant cell tumor of bone: oncological and functional results of long-term follow-up. Jpn J Clin Oncol. 1998 May;28(5):323-8. https://doi.org/10.1093/jjco/28.5.323. PMID: 9703860.
- Gillespie RJ, Levine A, Fitzgerald SJ, Kolaczko J, DeMaio M, Marcus RE, Cooperman DR. Gender differences in the anatomy of the distal femur. J Bone Joint Surg Br. 2011 Mar; 93(3):357-63. https://doi.org/10.1302/0301-620X.93B3.24708. PMID: 21357958.
- Hu Y, Zhao L, Zhang H, Yu X, Wang Z, Ye Z, Wu S, Guo S, Zhang G, Wang J, Ning X. Sex Differences in the Recur-rence Rate and Risk Factors for Primary Giant Cell Tumors Around the Knee in China. Sci Rep. 2016 Jun 20;6:28173. https://doi.org/10.1038/srep28173. PMID: 27321308; PMCID: PMC4913301.
- Hannah MK, Easterling EJ, Woodson CA. Giant Cell Tumor of the Distal Femur. J Orthop Sports Phys Ther. 2016 Nov;46(11):1011. https://doi.org/10.2519/jospt.2016.0419. PMID: 27802797.
- Ambrosi F, Righi A, Benini S, Magagnoli G, Chiaramonte I, Manfrini M, Gasbarrini A, Frisoni T, Gambarotti M. Giant Cell Tumor of Bone in Patients under 16 Years Old: A Single-Institution Case Series. Cancers (Basel). 2021 May 25;13(11):2585. https://doi.org/10.3390/cancers13112585. PMID: 34070432; PMCID: PMC8197501.
- Traub F, Singh J, Dickson BC, Leung S, Mohankumar R, Blackstein ME, Razak AR, Griffin AM, Ferguson PC, Wunder JS. Efficacy of denosumab in joint preservation for patients with giant cell tumour of the bone. Eur J Cancer. 2016 May; 59:1-12. https://doi.org/10.1016/j.ejca.2016.01.006. Epub 2016 Mar 15. PMID: 26990281.
- Suzuki Y, Nishida Y, Yamada Y, Tsukushi S, Sugiura H, Nakashima H, Ishiguro N. Re-operation results in osteoarthritic change of knee joints in patients with giant cell tumor of bone. Knee. 2007 Oct;14(5):369-74. https://doi.org/10.1016/j.knee.2007.05.008. Epub 2007 Jun 29. PMID: 17601737.
- Hosseinzadeh S, De Jesus O. Giant Cell Tumor. 2022 Aug 22. In: Stat Pearls [Internet]. Treasure Island (FL): Stat Pearls Publishing; 2022 Jan. PMID: 32644655.
ARTICLE TYPE: Case Report;
ORCID ID: Open Researcher and Contributor Identifier (ORCID) ID of corresponding author: https://orcid.org/0000-0002-9944-6250;
ETHICAL: Institutional ethical committee and prior patient consent obtained;
ACKNOWLEDGEMENT: None;
FINANCIAL DISCLOSURE: The authors declare that there was no financial aid received.;
CONFLICT OF INTEREST: No conflict of interest associated with this research work.;
AUTHORS CONTRIBUTION: Idea and Conceptualization: Dr SSS., Data Collection and editing: LK and SRV;
AUTHORS AFFILIATIONS: Dr. S.S. Subramanian, MPT, Ph.D., Principal and Dean, Sree Balaji College of Physiotherapy, Bharath Institute of Higher education and Research (BIHER), Chennai, India. Mrs. Lakshmiprabha K, MPT, Professor, Sree Balaji College of Physiotherapy, Bharath Institute of Higher education and Research (BIHER), Chennai, India. Ms. Shalini RV, MPT, Assistant Professor, Sree Balaji College of Physiotherapy, Bharath Institute of Higher education and Research (BIHER), Chennai, India.;
CORRESPONDING AUTHOR EMAIL: subramanian.deanphysio@bharathuniv.ac.in; subramanian.podhigai1968@gmail.com;
ARTICLE CITATION: Subramanian SS, Lakshmiprabha K, Shalini RV. Physiotherapy in post excision and curettage of giant cell tumour– evidence based case study. SALT J Sci Res Healthc. 2022 November 14; 2(2): 24-29.
PUBLISHER’S NOTE: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
